Around 17% of patients use United Healthcare insurance for their treatment here at Symetria. We are in-network with United Healthcare, work with them every day and know the insurance company well.
In This Article
Does United Healthcare Cover Substance Abuse Treatment?
Yes, most United Healthcare plans provide coverage for drug and alcohol use treatment, including inpatient and outpatient detox, MAT and therapy programs.
Whether a specific treatment is covered by UnitedHealthcare depends on the specific plan you or your employer chose and whether the addiction treatment provider is in-network with United Healthcare.
In-Network vs. Out-Of-Network United Healthcare Coverage
Some United Healthcare plans don’t cover out-of-network services at all, while others cover them but at a higher out-of-pocket cost.
- UnitedHealthcare Choice: Provides in-network coverage only, with no coverage for out-of-network providers.
- UnitedHealthcare Choice Plus: Offers savings for staying within the network but also provides some coverage for out-of-network providers.
- UnitedHealthcare Options PPO: This plan is more flexible and covers both in-network and out-of-network providers.
Symetria is an in-network provider with United Healthcare and can accept any of these United Healthcare plans, including Medicare plans.
How Much Does Addiction Treatment Cost with United Healthcare?
Covering treatment doesn’t mean United Healthcare pays for all of the treatment.
Your specific costs depend on your plan’s deductible, coinsurance, copayment and out-of-pocket maximum rates.
An employer can customize these rates however they want. Usually higher rates on these numbers means a lower monthly premium rate taken out of our paycheck and/or paid by your employer. There are hundreds of different rate combinations. If an employer offers multiple plans, the cheapest plan typically has less coverage.
United Healthcare Deductibles
Deductible is the amount you have to pay before insurance pays anything. Deductible amounts vary significantly and reset every year.
- A high deductible plan might be $1,400 for an individual or $3,000 for a family.
- More traditional plans might range from $500 to $1,500 for individual plans.
If you were hospitalized or accumulated other medical charges before seeking addiction treatment, then you might not have any deductible left to pay. If you also hit your out-of-pocket maximum or if your plan does not have co-insurance rates, then your addiction treatment would be free to you.
United Health Coinsurance
After meeting the deductible, most plans go to a coinsurance phase where you pay a percentage for healthcare and United Healthcare starts also paying a percentage.
- Typically, patients owe 10% to 40% of the treatment costs for co-insurance.
- An 80/20 split means that after you've met your deductible, the insurance would cover 80% of the cost of covered services, and you would pay 20%.
You pay continuance until you hit your out-of-pocket maximum.
United Health Out-of-Pocket Maximum
Out-of-Pocket Maximum means insurance pays the rest of your healthcare for the rest of the year and you owe nothing to the addiction treatment provider.
- OOP max rates are often around $3,000 to $8,000 for individual plans, usually higher for family plans.
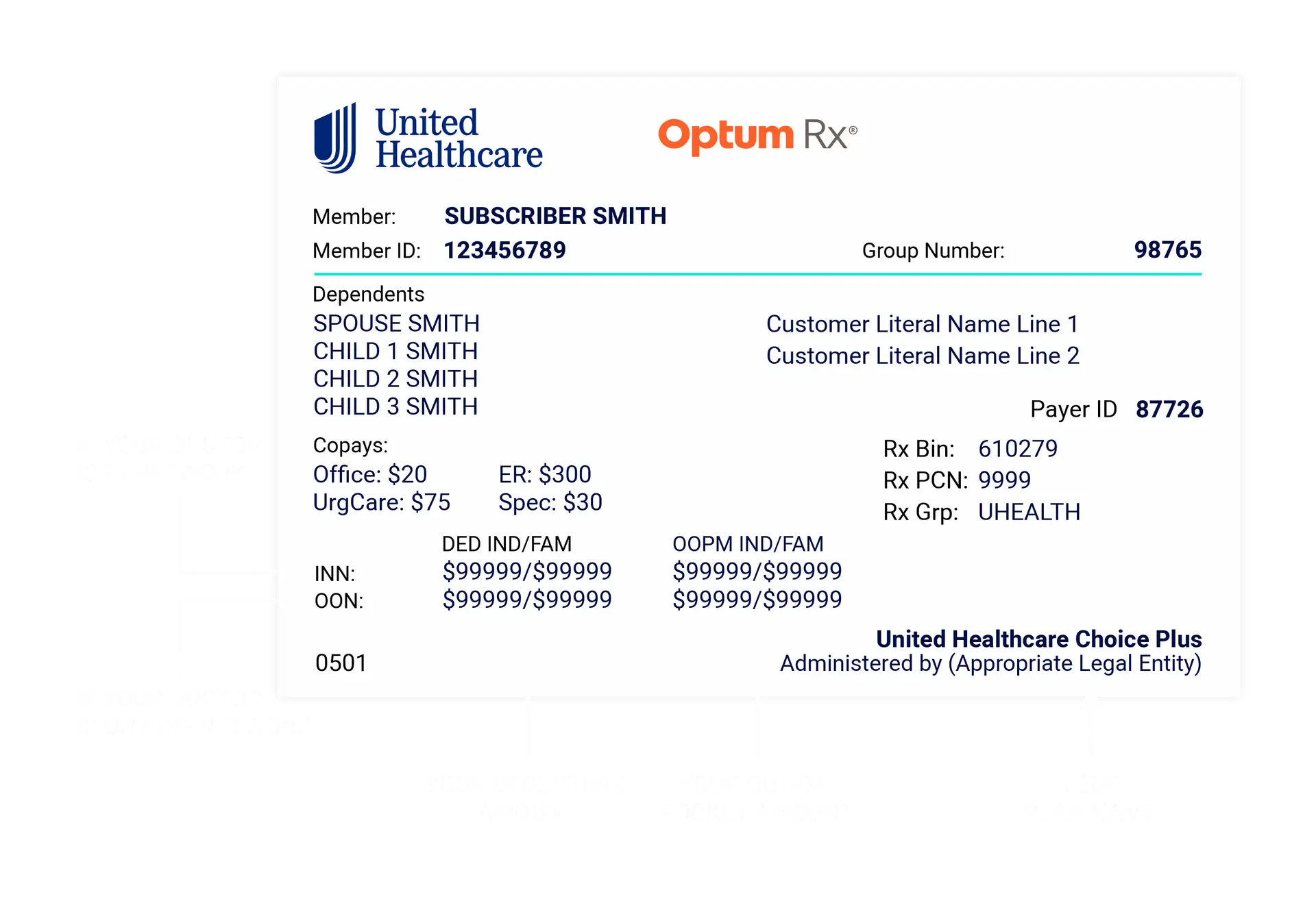
Reading Your United Health Card
Getting Cost Answers
An addiction treatment provider should talk to your insurance upfront and give you a cost estimate before you come in.
That way, your policy's deductible and out-of-pocket rates, as well as the healthcare costs you've already paid for the year can all be factored in.
You may also want to ask the provider directly and even consider checking with your insurance to ensure the provider is in-network. (I've seen out-of-network providers tell patients their treatment "is covered" without mentioning that it's out-of-network coverage which is almost always more expensive).
What kind of addiction treatment does United Healthcare Cover?
| Treatment Option | Covered by Most United Plans | Offered at Symetria |
| Inpatient Detox | ✓ | X |
| Inpatient Rehab | ✓ | X |
| Outpatient Detox | ✓ | ✓ |
| Intensive Outpatient Programs (IOP) | ✓ | ✓ |
| Outpatient Therapy | ✓ | ✓ |
| Methadone Treatment | ✓ | ✓ |
| Suboxone Treatment | ✓ | ✓ |
| Vivitrol / Naltrexone Treatment | ✓ | ✓ |
Does United Health Cover MAT?
While some plans may exclude MAT coverage, most UnitedHealthcare plans do cover Suboxone, Methadone and Vivitrol and the generic form of these medications, as well as any related office visits.
United Healthcare also generally covers any medications used to help with medication side effects or withdrawal symptoms like anxiety withdrawal insomnia.
UnitedHealthcare has a tiered system for prescription drugs to decide what is covered and the cost to the patient. These can vary by each specific plan, but generic versions of medications are more likely to be covered and cost less. ⓘ
Tier 1: Generic Drugs
- Coverage: These are usually covered at the highest level.
- Cost to Patient: Lowest coinsurance.
- Example: a patient might pay a copay of $10 for a month's supply.
Tier 2: Preferred Brand-Name Drugs
- Coverage: These drugs are covered but at a slightly lower level than Tier 1.
- Cost to Patient: Higher copayment or coinsurance than Tier 1.
- Example: The copay might range from $20 to $50 for a month's supply.
Tier 3: Non-Preferred Brand-Name Drugs
- Coverage: Lower coverage level compared to Tiers 1 and 2.
- Cost to Patient: Even higher copayment or coinsurance.
- Example: A patient might pay a copay of $50 to $100 or more, or a coinsurance rate like 40%.
Tier 4: Specialty Drugs
- Coverage: These drugs are often the most expensive and may be used for more complex conditions.
- Cost to Patient: Highest cost, often a coinsurance percentage rather than a fixed copay.
- Example: The patient might pay 25% to 50% of the drug's cost, which can be substantial for high-cost medications.
Does United Healthcare cover Suboxone?
Yes, Suboxone is covered by United Healthcare.
Many UnitedHealthcare plans classify Suboxone as a Tier 3 medication. But, generic buprenorphine/naloxone films are classified as Tier 1, which is usually less expensive to you and to United Healthcare.
At Symetria, patients tend to use generic Suboxone because it is preferred by insurance companies and your medication is bundled with your office visit here because the pharmacy is on-site. You don’t have to go elsewhere to get the medication.
United Healthcare covers whether used as a Suboxone tapper or maintenance. The insurance also covers Subutex (buprenorphine only) and Sublocade (suboxone injections).
Does United Healthcare cover methadone maintenance?
Yes, United Healthcare covers methadone maintenance! Not all methadone clinics accept insurance, but methadone treatment is covered by all major insurance companies including United Healthcare.
At Symetria, most methadone patients use insurance. The treatment here is very different from self-pay clinics.
Many people don't realize that methadone tapers, opioid detox and methadone maintenance dosing are all covered by all major insurance companies like Aetna, Cigna, Blue Cross Blue Shield and, of course, United Healthcare. Some methadone clinics choose not the accept insurance like Family Guidance Centers Chicago, but you don't have to self-pay.
Does United Healthcare Cover IOP Programs?
Generally, yes IOP is covered by United Healthcare.
Insurance companies set specific criteria for what constitutes IOP, which involves 3-hour sessions 3 times per week. If you are consistently not meeting United Healthcare's criteria for IOP, the IOP might not be covered. Providers should be staying in touch with you and your insurance to ensure and advocate for your coverage, but sadly this isn't always the case.
United Healthcare Detox & Rehab Coverage
Does United Healthcare cover drug rehab?
Yes, United Healthcare provides coverage for drug rehab, including both inpatient and outpatient options.
Outpatient options tend to be preferred by insurance companies like United Healthcare because outpatient treatment is cheaper for patients and research shows it is just as effective as going away to an inpatient rehab.
But, every circumstance is different. If you need help deciding what kind of treatment to choose, call (866) 955-2481. You can talk it through with a peer or schedule to meet with the doctor. The doctor can either get you started on outpatient treatment that day or make a referral for inpatient care, if that’s what is needed.
Does United Healthcare cover alcohol rehab?
Yes, United Healthcare covers alcohol rehab, including both inpatient and outpatient programs. Alcohol detox is typically recommended inpatient, which usually lasts 3-10 days. For there, treatment can continue inpatient or switch to outpatient. Either way, alcohol use treatment is covered by United Healthcare.
Does United Healthcare cover detox?
Yes, United Healthcare covers detox — whether in a hospital setting, an inpatient residential center or an outpatient clinic. Detox helps with the physical addiction and withdrawals. However, further treatment is recommended by all major health organizations — including the CDC, WHO and ASAM.
Other United Healthcare Addiction Treatment Coverage FAQs
How do I get reimbursed for addiction treatment I already paid for?
Some plans may require prior authorization or a referral to be covered. If this was not done ahead of time or if the provider is out-of-network and your plan only covers in-network providers, then the treatment costs would not be reimbursed.
Otherwise, to get reimbursed from UnitedHealthcare for addiction treatment you've already paid for, you'll need to submit a claim.
- Sign in to your UnitedHealthcare health plan account and go to the “Claims & Accounts” tab.
- Select “Submit a Claim” to download and print the Medical Claims Submission form.
- Complete all fields on the form and gather all claim receipts,
- Mail it to the address on your health plan ID card.
After processing, you'll receive an Explanation of Benefits (EOB) from UnitedHealthcare explaining the charges. If the claim is approved, UnitedHealthcare will reimburse you directly.
Are UnitedHealthcare, UnitedHealth Group and Optum the same?
UnitedHealth Group is the parent company.
UnitedHealthcare is the part of the company that provides health insurance. UnitedHealthcare works with employers and handles medical claims.
Optum is the part of the company that specializes in mental health and substance use disorder services. Optum is the branch within UnitedHealth Group that vetted Symetria Recovery when becoming an in-network provider. And, Optum employees are who we work with on a daily basis to help patients understand any costs for UnitedHealthcare plans.ⓘ
Does Symetria accept United Healthcare insurance?
Yes! United Healthcare is accepted for all services at any of our 13 locations across Illinois and Texas.
Substance Use Treatment In-Network with United Healthcare
Illinois Addiction Doctors
- Chicago Addiction Clinic
- Naperville Addiction Clinic
- Joliet Addiction Clinic
- Des Plaines Addiction Clinic
- Palos Heights Addiction Clinic
- Vernon Hills Addiction Clinic
Texas Addiction Doctors
- Houston Addiction Clinic
- Spring Addiction Clinic
- College Station Addiction Clinic
- Fort Worth Addiction Clinic
- Hurst Addiction Clinic
- Lewisville Addiction Clinic
- Arlington Addiction Clinic
If you are not in the Chicago, Fort Worth or Houston area, you can try searching on the UnitedHealthcare website directly. (Though only 1% of Symetria patients found Symetria that way. Most patients simply use Google).